As Sahiyo’s U.S. operations and programs have grown, we invited various individuals from a host of backgrounds and professions to join our U.S. Advisory Board. The advisory board provides strategic advice to the management of Sahiyo and ensures that we continue fulfilling our mission to empower communities to end female genital cutting and create positive social change through dialogue, education, and collaboration based on community involvement.
This month, we are pleased to highlight Joanne Golden who graciously serves as a member of our U.S. Advisory Board.
1) Can you tell us a bit about your background?
I was born and (mostly) raised in Massachusetts, but I got the travel bug at age 4, when my dad was in the U.S. Army and stationed at the Supreme Headquarters Allied Powers Europe (SHAPE) in Belgium. My mom, brother, and I were able to accompany him and we lived there for three years, where I attended school with children from other countries, learned about different cultures and languages, and traveled between most Western European countries (not Eastern Europe, as it was still during the Cold War). When I returned to the U.S., I knew my perspective was already broader than that of my peers and I became curious about history, politics, geography, and languages. I was determined to be the first female Secretary of State in the United States! Well, that didn’t happen, as Madeleine Albright beat me to it, and other opportunities came my way. I attended Boston University and received my Bachelor of Arts in International Relations with a minor in French (1990), spent my junior year abroad in Grenoble, France, and I was invited to my friend’s wedding in Egypt, where I spent six weeks as a guest of her family and friends. I could not have been happier!
My career trajectory did not go as planned as I moved towards financial services, rather than the foreign service, and I worked for 15 years at State Street Corporation in Massachusetts, during which I attended Boston University Graduate School of Management and received my Masters in Business Administration (1997). However, after serious reflection and research, in 2006, I decided to change the direction of my life and pursue a career in public service by going to law school, and I graduated with Pro Bono Honors from Suffolk University Law School in 2009 and was the 1st recipient of the Suffolk Law School Pro Bono Exemplary Service Award. During law school, I focused my electives on civil and human rights issues, particularly on human trafficking, children and women’s rights, for which I wrote a paper entitled “Impact of China’s One Child Policy and Cultural Gender Preference on Girl Child Discrimination and Mortality In China.” For a year after graduation, I worked with two NGOs and the Massachusetts Anti-Human Trafficking Coalition, in order to support state specific anti-human trafficking legislation, which went into effect in 2012, and to study the demand-side of sex trafficking. I am currently a federal attorney for the Social Security Administration’s Office of Hearing Operations since 2010, an active member of the Women’s Bar Association of Massachusetts (WBA). Since May 2013, I am part of a working group that researched, drafted, and advocates for state-level legislation to ban the practice of Female Genital Mutilation/Cutting (FGM/C) in Massachusetts.
I am also a fierce Boston sports fan. I study the Irish language and violin in what little time I have left over, and I recently got married to Greg, who regularly tells me how proud he is of the work I do.

2) When did you first get involved with Sahiyo and what opportunities have you been involved in?
I first became involved with Sahiyo about three years ago, through my interactions with Mariya Taher, who joined the WBA’s FGM/C legislative working group to help us advocate for state-level legislation to ban the practice of FGM/C in Massachusetts. I was introduced to Mariya on a monthly phone call led by Equality Now, which was trying to bring together a coalition of legal and medical experts, non-profits, federal and state law enforcement, and victim-survivors across the U.S. and between the U.S. and other countries, to eradicate FGM/C by 2030. Mariya brought valuable insight to our working group as a non-attorney, survivor, and founding member of Sahiyo. She showed us the human side and cost of FGM/C for girls and women. It is through Mariya that we made deeper contacts within the Bohra and Somali communities in Boston. We have new contacts with American-born women who are also cut, and we garnered more legislative support for the Massachusetts FGM/C bill with her testimony and willingness to tell such a deeply personal story. With Mariya and Sahiyo, we also successfully initiated a change.org petition to support the MA state legislation with over 300,000 signatures. I have admired her efforts to give a voice to girls and women through the Sahiyo Stories project. I also became a member of the Sahiyo U.S. Advisory board last year, and participated in our successful Boston FGM/C roundtable in April 2019.
3) How has your involvement impacted your life?
As I explained previously, in 2006, I decided to change the direction of my life and pursue a career in public service by going to law school. I followed my head, my heart, and my conscience to law school and focused on issues of civil rights, children and women’s rights, during my studies, but I could never have known that it would lead me here. When people ask me what I do, I always reply that I am an attorney for the federal government. But I also add that I fight for the rights of women and children against being trafficked and being irreparably harmed, physically and mentally, by FGM/C. I am proud and humbled by Sahiyo’s mission and that Mariya asked me and trusted me to be part of the Sahiyo U.S. Advisory Board.
4) What pieces of wisdom would you share with new volunteers or community members who are interested in supporting Sahiyo?
If you don’t know what you can do, then ask, “How can I help with this cause?” and someone will answer. Also, success is not a straight line from A to B. There are steps backward and forward, abrupt changes of direction, and even some side trips down a rabbit hole that you did not see coming. It is all necessary and all worth it. Be humble and open to what others have to teach you. Lean on each other for support. In my example, I had heard of FGM/C while I was in law school, but my focus and energy were on anti-human trafficking efforts and opportunities. Once the Massachusetts state human trafficking bill was passed in November 2011, and went into effect in 2012, I wondered, “Now what?” The answer did not come until May 2013 with the Women Bar Association’s FGM/C working group, and that group morphed as members came and went, but I feel our mission came into real focus after the first legislative session, in which our bill did NOT pass, as we expected it to. I was deflated at first, but then I met Mariya through Equality Now, and I was blown away with her advocacy experience. Mariya and Sahiyo clarified for me “who” we were advocating for, and I have learned how to be an advocate for change, and not just an arguer of legal facts because real change begins with people and the healthy, productive relationships you build in life. I am happy and proud of the relationships I have made within the Sahiyo community and with our mutual commitment to the full and equal participation of women under the law and in society by advocating for the abandonment of FGM/C in the U.S. and abroad.
——






 As I mentioned in my prior
As I mentioned in my prior 

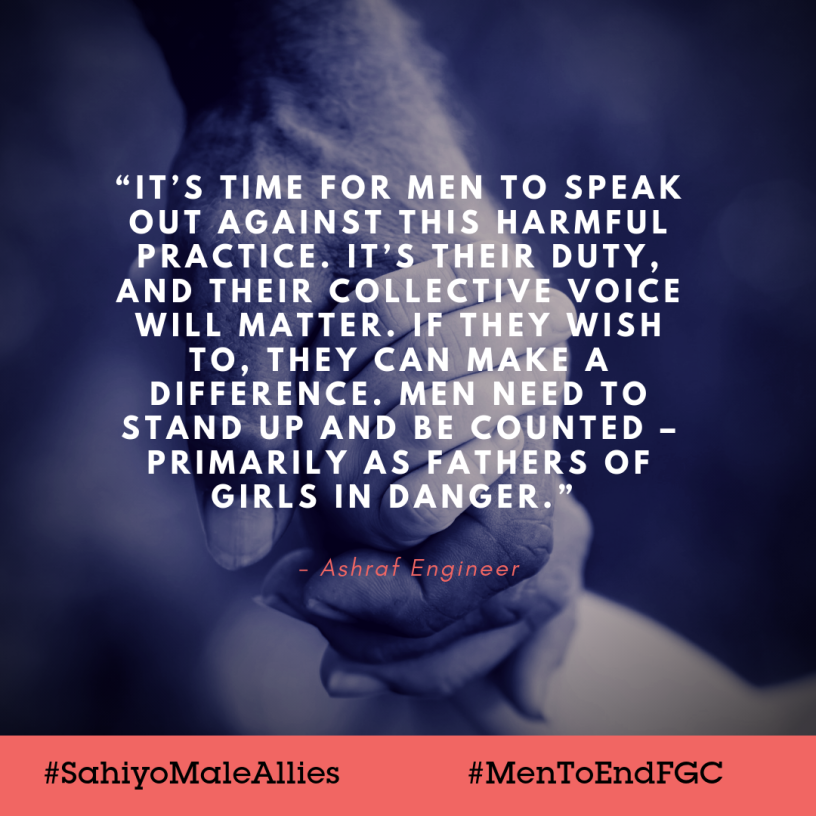 The issue of female genital cutting (FGC) is usually told from a woman’s perspective – for obvious reasons. Women around the world have spoken up against this practice that has gone on far too long, and we commend those who have made their voices heard. At Sahiyo, we know that while a lot of progress has been made, there is still a lot to be done to ensure that girls and women no longer undergo FGC. We know that more voices need to be heard, and that’s why we launched our male ally campaign.
The issue of female genital cutting (FGC) is usually told from a woman’s perspective – for obvious reasons. Women around the world have spoken up against this practice that has gone on far too long, and we commend those who have made their voices heard. At Sahiyo, we know that while a lot of progress has been made, there is still a lot to be done to ensure that girls and women no longer undergo FGC. We know that more voices need to be heard, and that’s why we launched our male ally campaign.